Dear HeartLogic™ users,
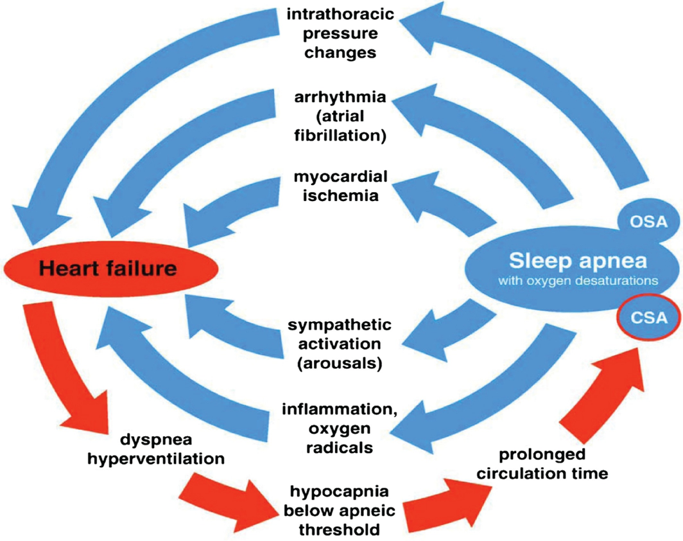
Comorbidities have great importance in HF and its management, in fact, as reported in current Guidelines for the Diagnosis and Treatment of Heart Failure (HF), they are key components of the holistic care of patients with HF. Sleep Apnea (SA) is a common comorbidity in HF, occurring in 30%–80% of affected patients, and has been shown to have a negative prognostic value in HF.
We are delighted to present you a recent publication from the DASAP-HF Study (The Diagnosis of Sleep Apnea in Patient With Heart Failure Study) about the correlation between cardiovascular events and the Respiratory Disturbance Index (RDI) computed by the ApneaScan™ algorithm.
In this issue you can also find a new Case Of The Month.
Heart Failure and Sleep Apnea
A high proportion of patients with HF and systolic dysfunction experience persistent and moderate-to-severe breathing disorders during nighttime and during short-term laboratory recording.
Clinical evidence demonstrates that HF patients with SA have an increased risk of mortality independent of traditional risk factors. Thus, diagnosing and treating apnea may become a relevant issue in the management of HF patients.
Although polysomnography is the diagnostic gold standard for SA, access to this procedure is limited and frequently a clinically significant SA remains undiagnosed1.
RDI is presented as a daily trend on remote device interrogation, together with the other diagnostic tools: HeartLogic index, contributing sensors, sleep incline sensor, trends of arrhythmias, etc.
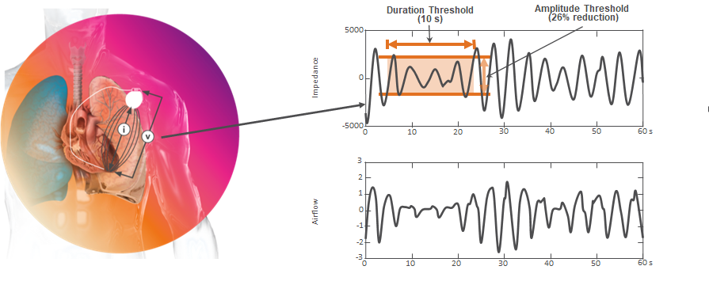
DASAP-HF Study
The short-term phase of the Diagnosis of Sleep Apnea in Patient with HF (DASAP-HF)2 study demonstrated that the RDI computed by the ApneaScan™ algorithm accurately predicts severe SA in patients who received an ICD or a CRT-D. Indeed, the average RDI value calculated by the ICD over a week period identified patients with severe disordered breathing (AHI≥30episodes/h) on the polygraphic recording subsequently performed, with 87% sensitivity and 56% specificity.
The aim of the recently published “Prognostic value of implantable defibrillator– computed respiratory disturbance index: The DASAP-HF study”, by Prof. G. Boriani et al3, was to investigate the association between the RDI values and the incidence of clinical events during the 24 months post-enrollment follow-up period.
Methods and Objective
The study was a prospective, non-randomized multicenter evaluation of patients implanted with an ICD or CRT-D having the ApneaScan diagnostic feature. Patients were enrolled and followed-up for 24 months to investigate the association between the RDI values and the incidence of clinical events: the endpoints were all-cause mortality and the composite of all-cause mortality or cardiovascular hospitalization.
One month after the enrollment, patients underwent a sleep study (unattended home nocturnal recording by means of a portable SA monitor).
In the analysis, the RDI calculated at one month after implantation was used to stratify patients (below or above 30 episodes/h).
Results
224 of the 265 enrolled patients, had a usable RDI and were considered for analysis.
SURVIVAL ANALYSIS
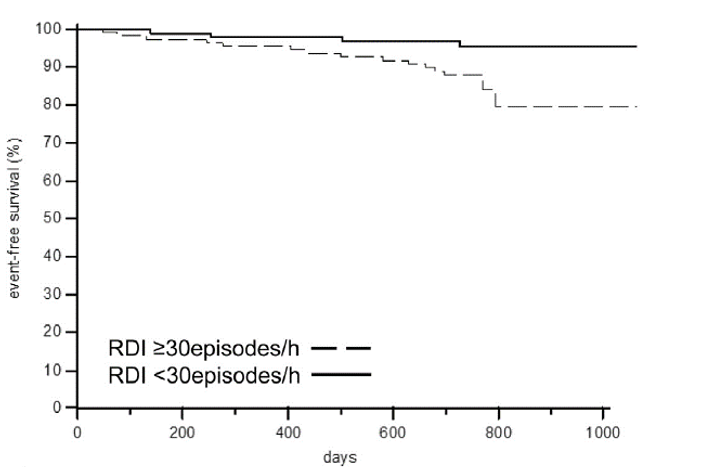
During a median follow-up of 25 months (25-75 percentile: 24-25 months) 19 patients died of any cause.
The Kaplan–Meier event-free curves (Fig. 1) for all-cause death, stratified by the presence or absence of ICD-detected severe SA, showed a marked separation, especially after more than one year of follow-up (log-rank test, p=0.023).
On multivariate analysis, RDI ≥ 30 episodes/h (HR 4.02; 95% CI 1.16–13.97; p= 0.029) and creatinine levels (HR 2.36; 95% CI 1.26–4.42; p=0.008) were found as independent predictors of death while SA detected at sleep study recording was not independently associated with an increased risk of death.
COMPOSITE ENDPOINT
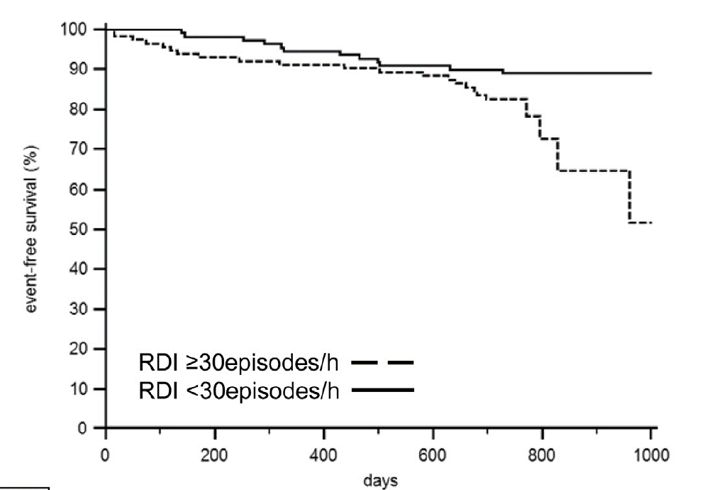
Cardiovascular hospitalizations were reported in 19 patients (8%) and 12 of them (5%) reported HF hospitalizations.
The combined endpoint of all-cause death or cardiovascular hospitalization occurred in 35 patients (16%).
The Kaplan-Meier curves are reported in Fig. 2 (long-rank test, p=0.048).
ADDITIONAL ANALYSIS
- Patients with ICD-detected SA showed lower ejection fraction and larger diastolic volumes at follow-up, but comparable functional status and quality of life.
- The proportion of patients clinically improved was lower (30% Vs 43%, p=0.049) in the group with RDI ≥ 30 episodes/h at 24-month follow up.
Conclusions
In HF patients implanted with an ICD, device-computed RDI accurately identifies severe SA.
This analysis demonstrated that higher RDI values are associated with an increased risk of death and cardiovascular events at a median follow up of more than 2 years.
- The ApneaScan™ algorithm may serve as an efficient tool for screening patients at risk of SA and as an independent predictor of all-cause death and cardiovascular hospitalizations in the long term.
- The availability of a reliable tool which allows automated detection of advanced SA may provide not only the possibility to closely track the benefit of treatments but also may provide further insights into the temporal relationship between apneic events and hemodynamic changes or arrhythmic events.
- In association with advanced Multisensor HF diagnostics like HeartLogic, ApneaScan™ may facilitate the management of cardiovascular risk factors and concomitant diseases, as suggested by current guidelines.
Case of the month
A VIGILANT CRT-D device was implanted in a heart failure patient. Six weeks later, the patient was evaluated during a standard follow-up and he reported to feel fine with no HF signs or symptoms.
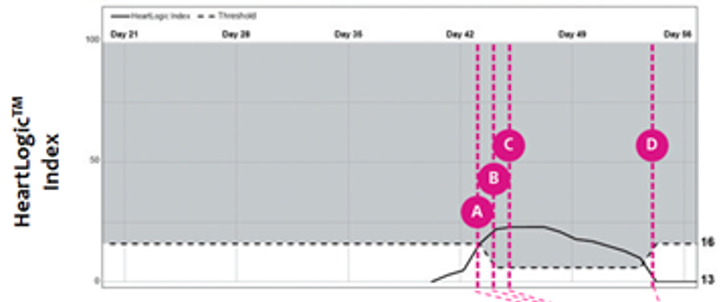
The day after the visit, an HeartLogic alert has been notified to the hospital…