Technique Spotlight:
EXALT™ Model D Single-Use Duodenoscope

Aditya Gutta, Stuart Sherman
MD, MD
Indiana University School of Medicine
Indianapolis, IN
Patient History

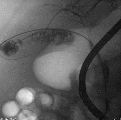
Major papilla partially within a duodenal diverticulum and with an indwelling endo-biliary stent. Biliary cannulation alongside the stent and subsequent stent removed with some stone extraction.
Scout film with biliary stent
Procedure
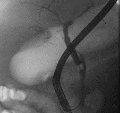
The patient was intubated and placed in a supine position. An EUS (Olympus, GF-UCT180) was done which showed findings consistent with chronic calcific pancreatitis (Rosemont criteria 9/9). Obstructive stones were noted in the main duct in the pancreatic body. Changes suggestive of mucin and a soft tissue lesion was noted in the genu of the pancreas. ERCP was subsequently performed with the EXALT™ Model D Single-Use Duodenoscope. No clear appearance of a fish-mouth orifice was seen on endoscopic examination of the pancreatic orifice. The main pancreatic duct was cannulated with a sphincterotome and guidewire (0.025 inch x 450 cm angled guidewire). Changes of severe chronic pancreatitis (Cambridge 5) were noted. The main duct in the pancreatic head contained filling defects suggestive of mucin. The pancreatic duct in the body of the pancreas and pancreatic duct in the tail of the pancreas contained multiple stones.
Educare
To explore in-depth physician-led lectures, procedural techniques and device tutorials, visit Educare.
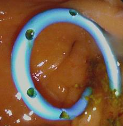
Get startedThe pancreatic duct was explored endoscopically using the SpyScope DS II direct visualization system and was advanced to the pancreatic body with excellent visibility. Diffuse frond/villous-like epithelium was noted in the main pancreatic duct in the head and genu of the pancreas with mucin floating in the duct. Fluid was aspirated through the SpyScope DS II for amylase concentration, cytology and CEA. The abnormal epithelium was biopsied with the SpyScope DS II directed SpyBite™ biopsy forceps. The pancreatic duct in the body of the pancreas contained a few stones. The SpyScope DS II was then withdrawn. The stones in the pancreatic body were then extracted with a stone-extraction balloon and basket.

Post Procedure
The patient did well in recovery post-procedure with no immediate post-procedure complications and was discharged as an outpatient. On a follow up phone call 2 weeks later, the patient was doing well with no delayed post-procedure complications. The results of the pancreatic juice analysis (CEA 13,807, Amylase 3,714) and biopsies of the duct epithelium were consistent with an IPMN. There was no high-grade dysplasia/malignancy on pathology. As per the family’s wishes, although there is a high risk of progression to malignancy and the definite treatment being surgery, given the patient’s advanced age and co-morbidities and given the very high risk of surgery compared the expected benefit, we elected not pursue aggressive interventions.
Discussion
This was a procedure with high complexity due to the following factors: advanced age of the patient; advanced maneuvers perfomed to diagnose a main PD-IPMN and successfully extract most of the main pancreatic duct stones. Pancreatoscopy with a SpyScope DS II, aspiration of pancreatic juice with the SpyScope DS II and SpyScope DS II directed SpyBite™ biopsy forceps of the mucinous epithelium of the main pancreatic duct was done. No immediate or delayed patient-related complications were noted.















