Dear HeartLogic™ users,
We know that this is a very tough period in all European countries due to Covid-19 emergency. We hope that you and your families, colleagues and patients remain well. We are grateful for your efforts in treating people affected by the virus and for continuing to ensure the best care to your heart failure patients.
The extraordinary measures taken to effectively serve the rapidly expanding patient population with Covid-19 but also to keep otherwise healthy patients away from the hospital and protect health care providers and caregivers can make access to care difficult for patients with heart failure routinely followed at your centers. We believe that for these patients HeartLogic may be the optimal solution to ensure continuous monitoring and early detection for prompt management of possible decompensation.
In this issue we would like to review with you assessment and treatment strategies in case of HeartLogic alert.
From the literature
The ESC Guidelines1 for Heart Failure diagnosis and treatment state that “patients with HF benefit from regular follow-up and monitoring of biomedical parameters to ensure the safety and optimal dosing of medicines and detect the development of complications or disease progression that may require a change in management” and suggest that Multiparameter monitoring based on ICD may be considered in symptomatic patients with HFrEF (LVEF ≤35%) in order to improve clinical outcomes. (Class of recommendation IIb, level of evidence B)
Several publications encourage remote monitoring, in order to efficiently optimize diagnostic and therapeutic pathways for cardiac implantable electronic device patients.
The recently published Position paper of the Italian Association of Arrhythmology and Cardiac Pacing2 on the intrahospital organization for remote monitoring of patients with CIEDs states that “…in case of clinical alert the patient is not moved, but the information concerning the patient is transferred: the patient himself remains physically at home and, in case of need, he is called to the referent hospital...”
The paper suggests that it is possible to improve the management of heart failure patients through the simultaneous analysis of several diagnostic parameters embedded in ICD/CRT-D devices.
And it reminds the critical points for effective remote monitoring of heart failure patients:
- patient's clinical knowledge
- daily alerts in clinical diagnostic monitoring
- multiparametric evaluation of clinical diagnostics
- presence of a multidisciplinary team dedicated to this activity
HeartLogic index meets the requirements of the ESC Guidelines. It allows an automatic analysis of multiple diagnostic sensors, it combines them into a single index and generates an alert in case of worsening heart failure.
Again, the HeartLogic index is the only validated (MultiSENSE study) and FDA approved tool for clinical use for heart failure monitoring.
The MANAGE-HF Study will generate evidence about the optimal guidelines to react to HeartLogic alerts. In the meantime, the current recommendations for the management of alerts are reported below.
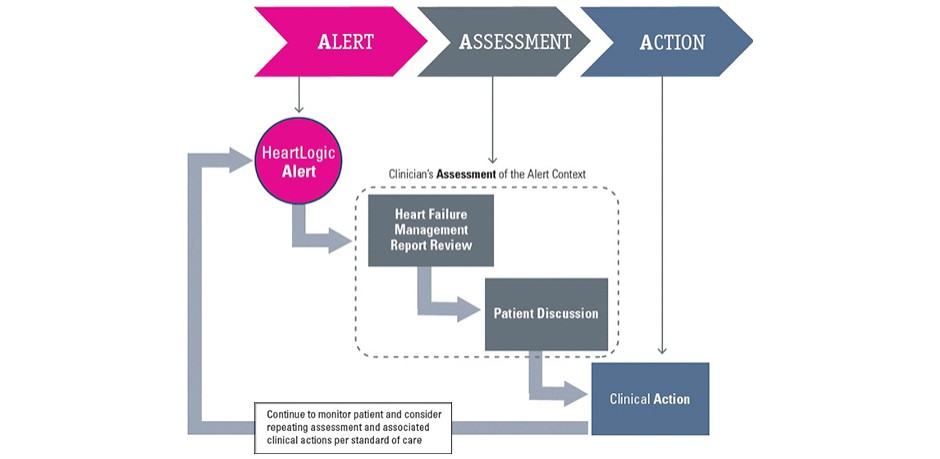
The 3A Process
The 3A Process is a clinical workflow proposed to allow detection of decompensation onset and to prevent further heart failure worsening.
Alert, Assessment and Action are the three main points of the flowchart reported below
Alert
The HeartLogic Index is computed daily and combines measurements from multiple device-based sensors, looking for changes from a historical baseline in a worsening direction and weighting those changes based on a patient’s current risk level.
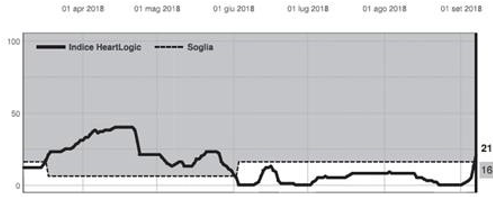
When the HeartLogic index crosses the threshold (nominal level 16) a yellow alert is notified (through LATITUDE™ website, mail or SMS text message) and the Heart Failure Management Report is available in the LATITUDE™ NXT Remote Patient Management System.
Assessment of patient clinical conditions
This step includes two main points: review the Heart Failure Management Report and contact the patient by phone to investigate his clinical condition and to identify potential causes of the alert.
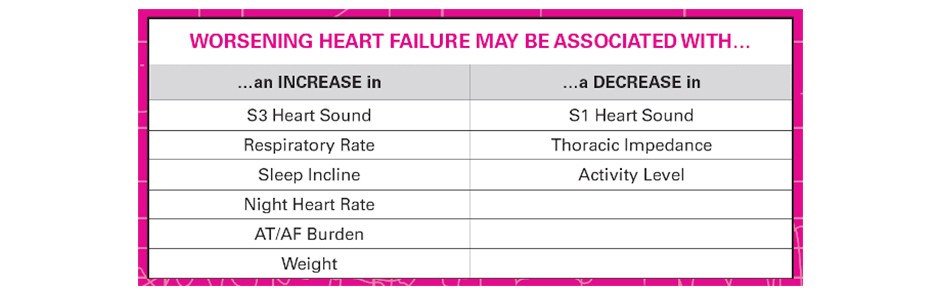
Review the Heart Failure Management Report: It is very important to analyze in depth all the daily trends for the management of heart failure: S3 heart sound, S1 heart sound, thoracic impedance, respiratory rate, night heart rate, sleep incline, activity level, AT/AF burden, V therapy, % LV paced and weight. This observation could help to better identify the nature of the alert and to determine the following actions.
In the table below are summarized the changes that can be associated to worsening heart failure
Contact the patient by phone and talk with him/her in order to assess the events that can be the causes of the alert and to identify signs or symptoms of decompensation.
During this conversation patient may be reassured, in order not to generate anxiety, but the context and all possible causes of the alert should be investigated:
1. Are there any factors that may have contributed to the alert, such as:
- Medication nonadherence
- Dietary indiscretion
- Use of harmful medications such as NSAIDs
- Recent medication changes
- Recent clinical events especially those requiring infusion of fluids (e.g., a surgery)
- Active ischemia
- Non-optimal medical therapy
Check on LATITUDE™ NXT Remote Patient Management System:
- Arrhythmia and device therapy (ATP, shocks)
- Reduction or loss of CRT (for patients with CRT devices only)
2. Are there other signs or symptoms of worsening heart failure, such as:
- Shortness of breath with exertion and/or at rest
- Shortness of breath when lying flat (orthopnea or paroxysmal nocturnal dyspnea)
- Sleeping regularly in a chair or on multiple pillows in bed
- Dry cough or frothy sputum
- Weight gain
- Swelling of abdomen, feet or ankles
- Changes in the frequency of urination
- Fatigue
Action
After patient discussion, consider treatment modifications in order to avoid worsening heart failure or to reduce patient signs and symptoms.
Based on the factors that could have contributed to the HeartLogic alert, different actions can be considered:
• Reinforce medication compliance
• Repeat patient education on dietary sodium and fluid restriction, remind of daily activity/exercise plan and, if possible, keeping regular follow-up appointments with his/her healthcare provider
• Address patient therapy related issues, such as worsening atrial burden, loss of CRT pacing, ventricular arrhythmias, etc.
• Treat fluid overload
• Further optimize current ESC guideline-directed medical therapies1
Monitoring of the patient should be continued to evaluate the evolution of the clinical condition. In particular, for patients who experienced an HeartLogic alert, closer follow-up could be considered.
Case of the month
A 80 year-old man underwent implantation of PERCIVA™ ICD VR for primary prevention of sudden cardiac death on December, 19 2017 and HeartLogic™ index was activated immediately after implantation.
After implantation the patient was fine till March, 17 2018, when…