Bone resources
ICE Cryoablation Technology
Overview
Patient information
The MOTION study
Cryoablation for Palliation of Painful Bone Metastases: The MOTION Multicenter Study
This multicenter, prospective, single arm, phase II study examined the impact of the treatment of a painful bone metastatic lesion in each patient.
Study objective
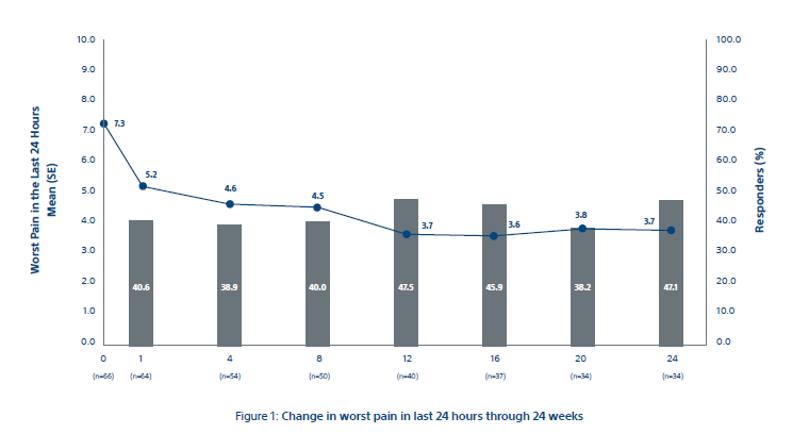
- The primary objective was to evaluate the efficacy of cryoablation for pain palliation of bone metastases from baseline to 8 weeks after cryoablation in worst pain in the last 24 hours.
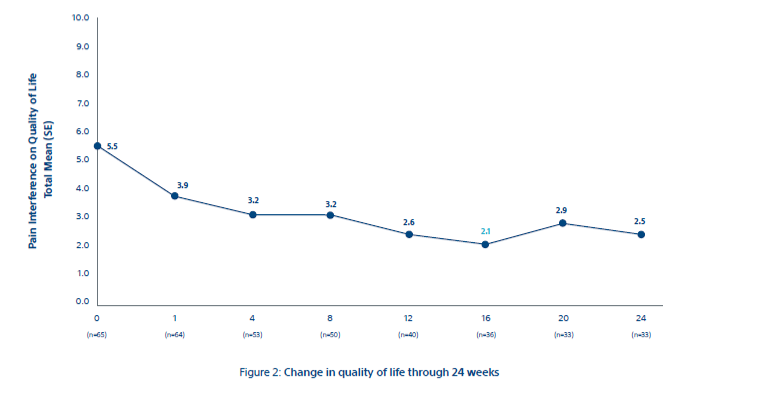
- Separate evaluations of ancillary efficacy endpoints were also made through 24 weeks.
Key results
The primary efficacy endpoint of mean change in worst pain in last 24 hours from baseline to week 8 was 2.61 ± 0.43 points (95% CI: -3.45, -1.78) as shown in Figure 1. Clinically meaningful changes from baseline were observed at all time points after week 8. In the completed case analysis (n = 64), mean pain scores improved by 2 points as early as week 1 and continued through week 24 and the 92% of participants achieved palliation (59/64), with median time to maximal pain relief of 39.0 days (95% CI: 43.7, 72.4 days; n = 59). Most participants achieved their maximum palliation by week 1 (33.9%; 20 of 59), week 4 (25.4%; 15 of 59), or week 12 (15.3%; nine of 59).
MOTION study conclusion
Overall, the data shows a rapid and durable pain relief along with a decrease in MEDD and a corresponding increase in the quality of life for patients.
Resources
EDUCARE
Boston Scientific clinical training for interventional radiologists
Our EDUCARE platform gives you instant, online access to a wealth of clinical education and training resources including continuing education courses. Explore training and education programs to help you succeed in providing the best patient care possible.