Calcium Prevalence & Rotational Atherectomy
Calcium is more common than you think. In the United States, over 30% of all patients treated for Percutaneous coronary intervention (PCI) present with some degree of calcium.
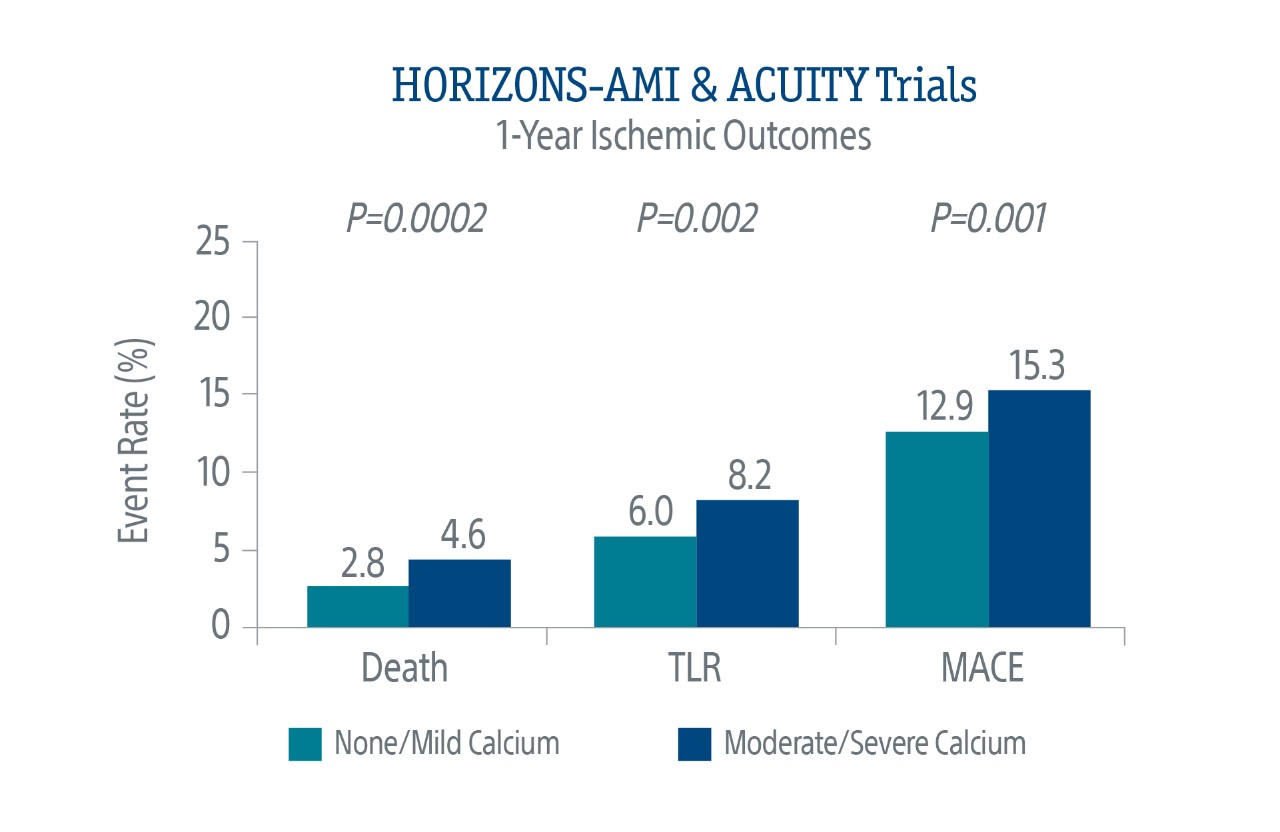
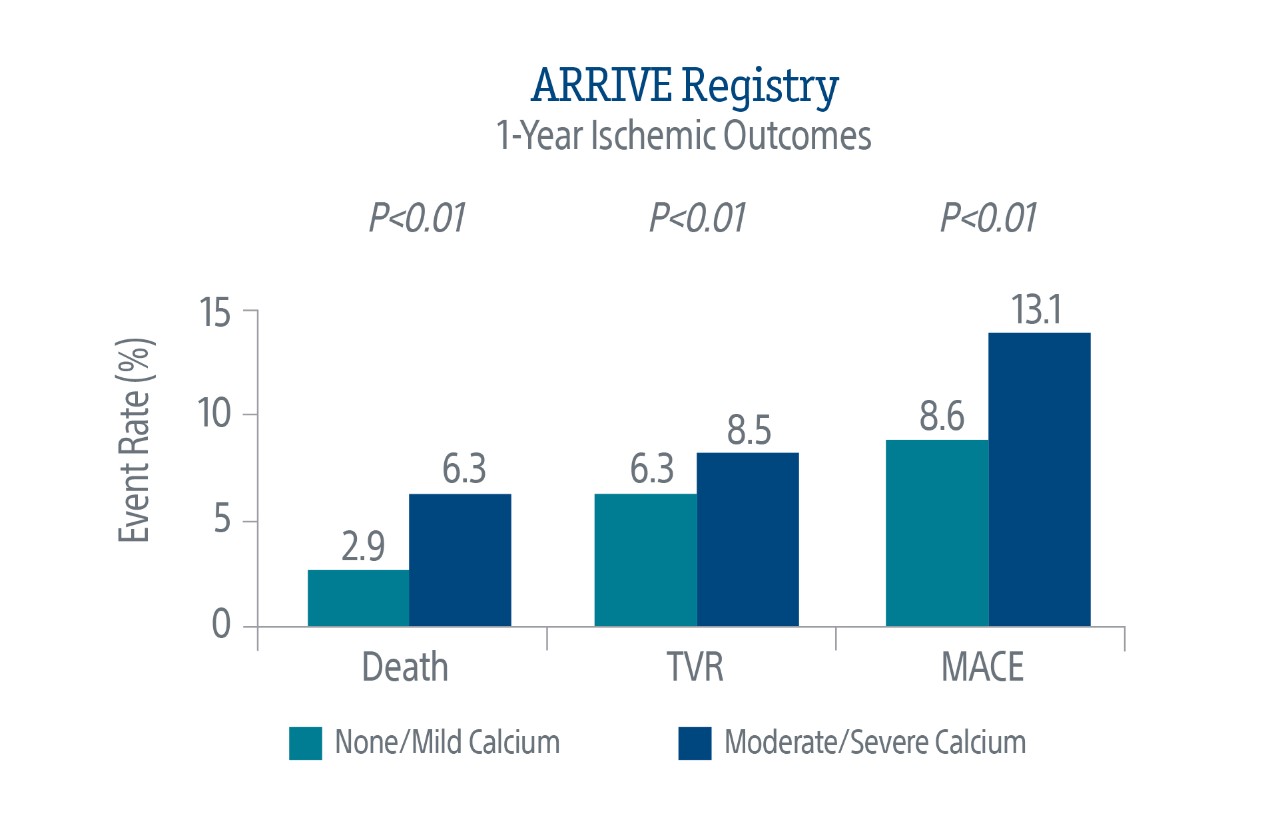
Calcium Impacts Long-Term Outcomes
Calcium is a growing problem in the treatment of coronary artery disease. Angiographic evidence indicates a high presence of target lesion calcification in patients undergoing PCI.1
Patients with calcium tend to be older with a higher prevalence of hypertension, kidney disease, previous CABG, and congestive heart failure.
Data Supports Rotational Atherectomy
A 2015 large, multicenter registry evaluated the outcomes of patients undergoing rotational atherectomy (RA) in 9 major Australian hospitals over an 8-year period (16,410 non-RA PCIs, 167 RA PCIs).3
In the RA cohort:
- Patients were more likely to be older with a higher prevalence of comorbidities
- Patients were more likely to have complex type B2 and C lesions
- 37% of patients had a previously failed PCI
These patients represented the most complex of the PCI population where no other interventional therapy was an option.
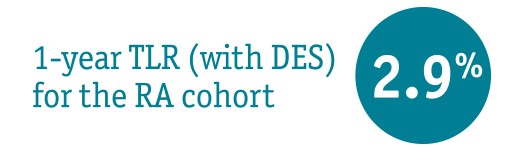
Study Findings: Rotational atherectomy was safe and effective in resistant lesions
When lesions treated with drug eluted stents (DES) (excluding bare metal stents) were isolated, analysis of the multicenter registry revealed a TLR rate of 2.9%.